Cholesterol: Myths & Reality
There is a lot of confusion about these little molecules. The one clear thing is that almost every doctor wants to drop the total cholesterol as low as possible and to take the LDL down to nearly nonexistent.
LDL: The “Bad Cholesterol.” Not all LDL is the same. Did you know there are Large LDL, IDL, VLDL, and sdLDL? They each have unique characteristics. Also, the LDL-C measured on the standard lipid panel is simply a weight measure of the LDL (mg/dl). It does not differentiate whether most of it is large or small. Large LDL works very efficiently and is much less worrisome than small-type LDL. Shouldn’t we know what we’re dealing with before jumping to conclusions?
The 2nd image is of an LDL Molecule attaching to an LDL receptor. If LDL is so bad, why would our body create it? Was it designed to kill us? Cause heart disease with critical blockages in our arteries? Why do our blood vessel walls have receptors for something so sinister? Maybe LDL plays an important role in the body, and we should not attempt to annihilate it?
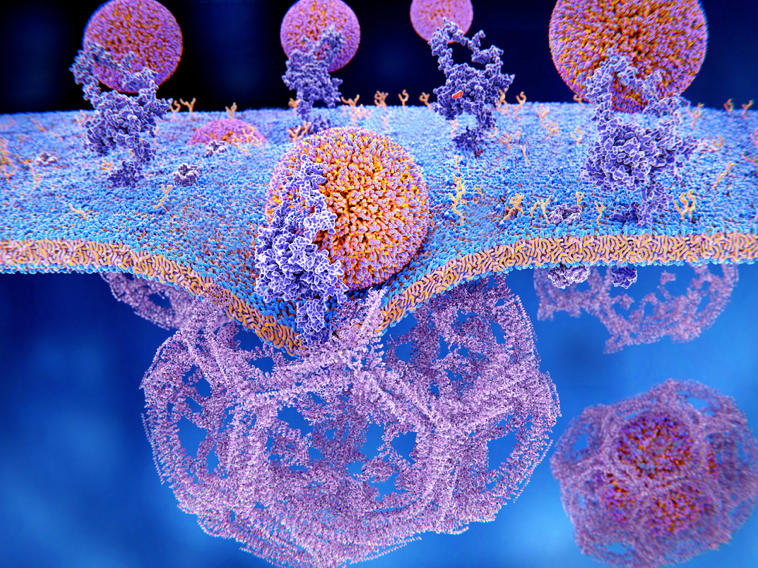
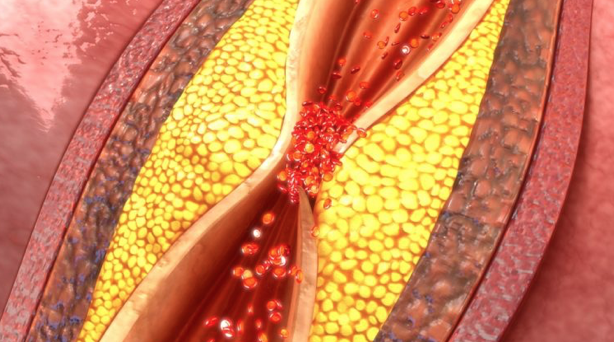
Were you aware that we do not eat LDL, but rather our liver produces it? It is our liver that determines the size and makeup of the LDL created (Large, Small, and everything in between). The liver responds to the environment around it. A pro-inflammatory environment (highly-processed diet, high-stress lifestyle, insulin resistance) leads to the production of more small LDL. A healthy diet and lifestyle result in larger LDL. A diet loaded with items from image 3 is a known cardiac risk factor because it leads to inflammation and insulin resistance.

We are now familiar with the process of Oxidation. This is something that occurs with digestion and inflammation (rusting). Oxidized LDL is more likely to get trapped in an artery and contribute to plaque formation. Small LDL is highly prone to oxidation, whereas Large LDL is not. We can measure the level of oxidized LDL in the bloodstream, providing a clearer picture of future risk.
HDL: the “Good” cholesterol. It holds the role of returning used-up cholesterol from the body back to the liver for recycling or elimination. Interestingly, there is also Large and Small HDL. An inflammatory diet and lifestyle lead to more production of small-type HDL, a far less efficient carrier. If most of the HDL is small, then Reverse Cholesterol Transport is sluggish. So often, little attention is paid to the low-normal HDL on the standard Lipid Panel (weight), and it is unlikely that you are having a measurement of the HDL Particle Number, let alone its size. But why would this matter, after all? Statins do not affect HDL.
Were you aware that you can have a High level of HDL and still be at increased risk for a heart attack? A High HDL-C does not tell us what type of HDL you are producing. The majority can still be small HDL, which is less protective and an increased risk. False reassurance.
STATINS: They reduce LDL production by the liver. They block the enzyme in the liver that leads to LDL production (HMG CoA Reductase). So, they reduce Total Cholesterol by lowering LDL-C (weight), and they do reduce the LDL particle number (LDL-P). What they do not do is change what type of LDL the liver is producing. If you continue with the same diet and lifestyle that leads to a high fraction of small LDL, you will still maintain a high fraction of small LDL; there will just be less of it.
Statins also do not affect the oxidation process that leads to damaged LDL in the circulation. Translation: There is still damaged LDL circulating that can get trapped in the inflammatory mess inside an artery and lead to plaque formation and increased risk for a heart attack. This could be why so many people on statins still get heart attacks? They do not address the root causes of inflammation – the real reason for atherosclerosis (plaque) in the first place.
Other Markers: There are other markers that are helpful in risk stratification for heart disease.
- High sensitivity CRP is a well-established one and is a marker of systemic inflammation.
- LpPLA2
- Myeloperoxidase
- ApoA1
- ApoB-100
- Lp(a)
ApoB is now becoming the new target (love-child) as the best indicator for heart attack risk. It is felt to be a better indicator than any other marker at this time. The truth is they all matter. They are all independent cardiac risk factors and reflect an imbalance in the body. There will be more that come to the forefront in the future.
None of them should be a clear indication for a medication. They are useful to tell us there is a problem that can be addressed. They reflect Inflammation, Insulin Resistance, Metabolic Syndrome, and HPA Axis Dysregulation, with thousands of potential root causes. Most of my colleagues, on hearing some of these words, would immediately conclude the need for Statin therapy, Metformin, Steroids, and Biologics. They do not address the real problem, and they will not prevent the outcome – most will create new ones.
If you have a heart attack, then the train has arrived at the station. You need a stent or bypass surgery. There is little question about this, and these are lifesaving and will improve the quality of life after. There will be medications that come with this. But what if you could make changes that slowed the train or turned it around? What if you could do something to prevent another heart attack (more stents, more dead heart muscle)?

The answer is quite simple, but it requires far more effort on your part. Most people, sadly, are not willing to make the necessary changes.
If you are interested in this type of testing, a risk assessment, and learning ways to reduce the risk, please feel free to contact us for a consultation.
Call us at (828) 536-0320 or
Email us at contact@optimalhealthwnc.net
